Report certain cases of viral hepatitis.
To report, call the reporting line.
- Within 24 hours—acute hepatitis A, B or E.
- Within 3 days—hepatitis C (acute), hepatitis D (acute or chronic) and pregnant women who test positive for hepatitis B surface antigen.
- Monthly—newly diagnosed chronic hepatitis B or C.
Testing
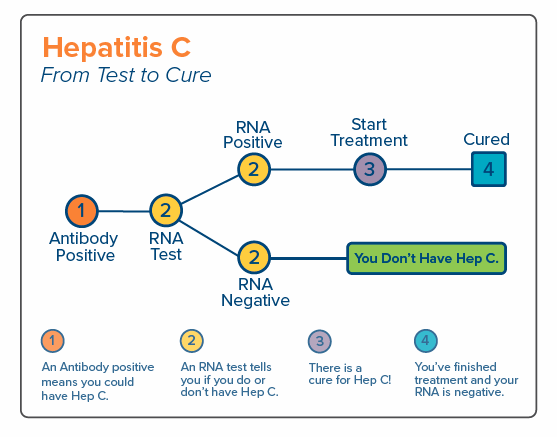
Hepatitis C
- Hepatitis C Information For the Health Professional (CDC).
- General Hepatitis C information (CDC).
- HCV Screening and Testing Guidelines—Screening and testing sequence resources from CDC and AASLD.
- Interpretation of Test Results for Hepatitis C Virus (HCV) Infection (CDC).
Testing and Vaccination
Hepatitis B
- The Impact of Nail Salon Industry Policies and Regulations (Hepatitis B Foundation).
- Hepatitis B Information For the Health Professional (CDC).
- General Hepatitis B information (CDC).
- Interpretation of Hepatitis B Serologic Test Results (CDC).
- Recommendations for Routine Testing and Follow-up for Chronic Hepatitis B Virus (HBV) Infection (CDC).
- Testing Asian-Americans and Pacific-Islanders (AAPI) for Hepatitis B (CDC).
- Screening Pregnant Women for Hepatitis B Virus (HBV) Infection (CDC).
- Hepatitis B stories.
Customizable wallet card for patients with information on testing, status, treatment, and prevention.
Customizable wallet cards for patients [Adapted from Philadelphia Department of Public Health]
Perinatal
Notify us of a pregnant woman with positive hepatitis C results or the birth of an exposed infant. To report, call reporting line.
- Screening Pregnant Women for Hepatitis B Virus (HBV) Infection (CDC – see page 2)
- Perinatal Hepatitis B: Guidelines for Prenatal Care
- Caring for Infants Born to Hepatitis B-Infected Mothers
Surveillance
- epiTrends: Hepatitis C Surveillance and Information (DOH)
- Chronic Hepatitis B and C Surveillance Report—summary of cases reported, December 2000-2011.
- Viral Hepatitis in Washington State 2016
Resources and Links
Hepatitis Elimination
- Mapping Hepatitis Elimination in Action—We’re on the map! See what we and other health departments are doing to eliminate hepatitis B and C.
- Washington’s Plan to Eliminate hepatitis C.
- National Strategy for the Elimination of Hepatitis B and C—Phase 2 report.
- National Viral Hepatitis Action Plan 2017-2020.
- The World Health Organization’s plan—Eliminate hepatitis B and C by 2030.
Washington State Department of Health
- epiTRENDS: A Monthly Bulletin on Epidemiology and Public Health Practice in Washington.
- Chronic Hepatitis B and C Surveillance Report—summary of cases reported, December 2000-2011.
- Washington State Department of Health: Hepatitis Information—for the public.
- Viral Hepatitis in Washington State 2016
State and National Hepatitis Organizations
- Hepatitis Education Project —provides educational materials and support for patients with hepatitis.
- Hepatitis C Online – addresses diagnosis, monitoring and management of hepatitis C virus infection.
Vulnerable Populations
- Asian and Pacific Islanders—Population risk for hepatitis B, barriers to screening, vaccination promotion and strategies to engage Asian communities.
- Men Who Have Sex with Men (MSM)—Risks of getting sexually transmitted diseases, including hepatitis A and B.
- People Who Use Injection Drugs—Risks for hepatitis B and C infection through the sharing of needles and drug-preparation equipment.
Viral Hepatitis in Specific Settings
- Healthcare Settings and Viral Hepatitis—discusses the risk of exposure and transmission of hepatitis B and C. Additional information is found on the Hepatitis in Healthcare Settings
- Correctional Facilities and Viral Hepatitis—describes the risk of incarcerated persons for acquiring hepatitis B and C. Additional information can be found on the Correctional Health link.
- Diabetes and Viral Hepatitis—discusses the risk of viral hepatitis infection in long-term care (LTC) facilities that are related to sharing of blood glucose monitoring devices.
Professional Articles
- Prevention of Hepatitis A Through Active or Passive Immunity—recommendations of the ACIP MMWR 2006; 55 (RR-7)
- Recommendations for Identification and Public Health Management of Persons with Chronic Hepatitis B Virus Infection—MMWR 2008; 57 (RR-8)
- A Comprehensive Immunization Strategy to Eliminate Transmission of Hepatitis B Virus Infection in the United States—recommendations of the ACIP Part 1: Immunization of Infants, Children, and Adolescents. MMWR 2005:54 (RR-16)
- A Comprehensive Immunization Strategy to Eliminate Transmission of Hepatitis B Virus Infection in the United States—recommendations of the ACIP Part II: Immunization of Adults. MMWR 2006; 55 (RR-16)
- Recommendations for the Identification of Chronic Hepatitis C Virus Infection Among Persons Born During 1945–1965—MMWR 2012; 61(RR-4)